Introduction
Prescription drug abuse has become a significant public health crisis worldwide, particularly in countries like the United States. The misuse of opioids, benzodiazepines, stimulants, and other controlled substances has led to increased addiction rates, overdose deaths, and societal costs. According to the CDC, over 100,000 Americans died from drug overdoses in a recent year, with prescription drugs being a substantial contributor.
In response, healthcare systems are leveraging advancements in Health Information Technology (Health IT) to address this epidemic. From electronic health records (EHRs) and Prescription Drug Monitoring Programs (PDMPs) to clinical decision support systems (CDSS) and telehealth, technology offers tools to improve prescribing practices, monitor patient use, prevent diversion, and enhance treatment outcomes.
This comprehensive discussion explores how Health IT is transforming efforts to combat prescription drug abuse, highlighting current technologies, their impact, challenges, and future prospects.
1. The Scope of the Prescription Drug Abuse Epidemic
1.1. Prevalence and Impact
Prescription drug misuse occurs when patients take medications in a manner not intended, such as taking higher doses, using someone else’s medication, or using medication for non-medical reasons. The consequences include dependency, overdose, and transition to illicit drugs like heroin.
1.2. Key Substance Classes Involved
- Opioids: Morphine, oxycodone, hydrocodone, fentanyl
- Benzodiazepines: Valium, Xanax, Ativan
- Stimulants: Adderall, Ritalin
- Others: Sedatives, muscle relaxants
1.3. Factors Contributing to the Epidemic
- Overprescription and lack of oversight
- Patient demand and misuse
- Diversion for illicit sale
- Inadequate monitoring systems
2. The Role of Health IT in Addressing Prescription Drug Abuse
Health IT encompasses a broad range of digital tools that facilitate data collection, analysis, communication, and clinical decision-making. Its application in combating prescription drug abuse includes:
- Improving prescribing safety
- Monitoring patient medication use
- Detecting diversion and doctor-shopping
- Enhancing patient education
- Facilitating coordinated care
3. Key Technologies and Strategies in Health IT
3.1. Electronic Health Records (EHRs)
EHRs are digital versions of patients’ medical histories. They enable providers to access comprehensive, real-time data, which aids in making informed prescribing decisions and tracking patient medication histories.
Impact:
- Reduce duplicate prescriptions
- Alert providers to prior opioid or controlled substance prescriptions
- Improve documentation of indications and contraindications
3.2. Prescription Drug Monitoring Programs (PDMPs)
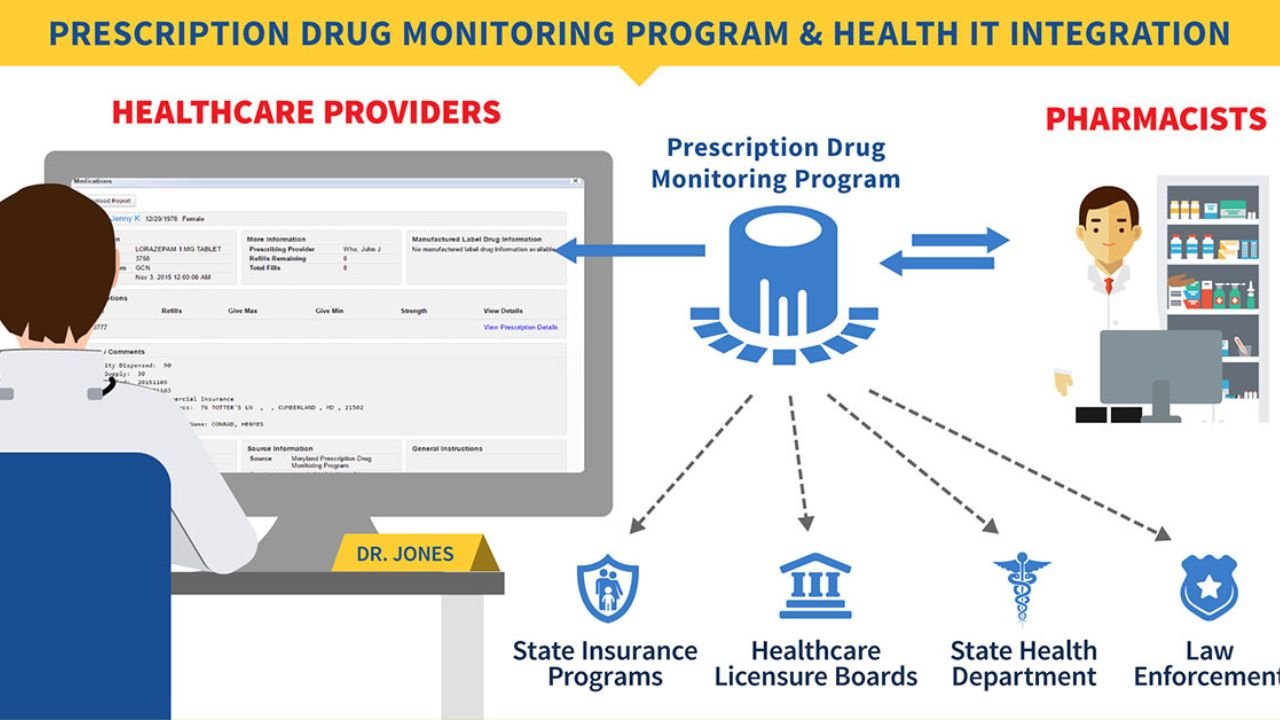
PDMPs are state-run electronic databases that track controlled substance prescriptions. Providers and pharmacists access PDMPs to review patients’ prescription histories before dispensing or prescribing.
Features:
- Real-time or near-real-time data
- Alerts for suspicious patterns
- Integration with EHR systems for seamless access
Benefits:
- Reduce doctor-shopping
- Identify patients at risk of overdose
- Inform safer prescribing practices
3.3. Clinical Decision Support Systems (CDSS)
CDSS are embedded within EHRs and other clinical platforms, offering alerts, reminders, and guidelines based on patient data.
Applications:
- Flag high-dose prescriptions
- Warn about drug interactions
- Provide guidelines for opioid prescribing and tapering
3.4. Interoperability and Data Sharing
Enabling different health IT systems to communicate ensures comprehensive patient data, including PDMP information, is accessible across providers, reducing fragmentation.
3.5. Telehealth and Remote Monitoring
Telemedicine facilitates access to addiction treatment, counseling, and follow-up care, especially for underserved populations.
Remote Monitoring Devices:
- Pill dispensers with tracking
- Wearables detecting physiological signs of overdose
- Apps for medication adherence and reporting
3.6. Natural Language Processing (NLP) and Big Data Analytics
Advanced analytics can identify patterns of misuse, risk factors, and emerging trends through large datasets, enabling proactive interventions.
4. How Health IT is Impacting the Fight Against Prescription Drug Abuse
4.1. Enhanced Prescribing Safety
Studies have shown that integrating PDMPs with EHRs reduces inappropriate prescribing. Providers can verify previous medication histories efficiently, decreasing overprescription and doctor-shopping.
4.2. Early Detection and Intervention
Health IT tools can identify patients at risk of misuse or overdose by analyzing prescription patterns. Alerts prompt clinicians to consider alternative treatments or refer patients for addiction services.
4.3. Reducing Diversion and Abuse
Real-time alerts help pharmacists and providers prevent diversion by flagging suspicious behaviors, such as early refill requests or overlapping prescriptions.
4.4. Improving Patient Outcomes
Electronic alerts support appropriate tapering protocols, reducing dependence. Telehealth expands access to addiction treatment, reducing barriers to care.
4.5. Data-Driven Policy and Public Health Responses
Aggregated data from PDMPs and other systems inform policymakers about trends, hotspots, and effectiveness of interventions, enabling targeted strategies.
5. Case Studies and Examples
5.1. State PDMPs and Their Effectiveness
- California’s CURES: After integrating PDMP data into EHRs, the state observed a significant decline in opioid prescriptions and doctor-shopping.
- Kentucky’s KASPER: Statewide implementation led to a reduction in high-dose opioid prescribing and overdose deaths.
5.2. Integrated EHR and PDMP Solutions
Some healthcare systems have embedded PDMP access directly into their EHRs, allowing clinicians to view prescription histories without leaving their workflow, increasing usage and impact.
5.3. Telehealth Initiatives
The COVID-19 pandemic accelerated telehealth use for addiction treatment, with regulations temporarily eased to permit remote prescribing of controlled substances under supervision.
6. Challenges and Barriers to Implementation
6.1. Data Privacy and Security
Ensuring patient confidentiality while sharing sensitive data across platforms remains a concern, requiring robust cybersecurity measures.
6.2. Interoperability Issues
Many systems are incompatible, hindering seamless data exchange. Standardization efforts are ongoing but still face obstacles.
6.3. Provider Engagement and Compliance
Clinicians may not consistently access or utilize PDMPs due to workflow issues, lack of awareness, or skepticism about efficacy.
6.4. Technical and Financial Barriers
Implementing sophisticated Health IT systems requires significant investments, technical expertise, and ongoing maintenance.
6.5. Legal and Regulatory Variations
Differing state laws regarding PDMPs, prescribing regulations, and data sharing complicate cross-state initiatives.
7. Future Directions and Innovations
7.1. Artificial Intelligence (AI) and Machine Learning
AI algorithms can predict patients at risk of misuse, enabling preemptive interventions.
7.2. Enhanced Data Analytics
Big data analytics can identify epidemic trends, inform public health campaigns, and optimize resource allocation.
7.3. Patient-Centered Technologies
Mobile apps and wearables can promote medication adherence, track usage, and alert users to risks.
7.4. Blockchain for Secure Data Sharing
Blockchain technology promises secure, decentralized data sharing across providers, pharmacies, and public health agencies.
7.5. Policy and Regulatory Support
Ongoing legislative efforts aim to standardize PDMPs and incentivize adoption of best practices.
8. Ethical and Social Considerations
Implementing Health IT solutions raises questions about patient privacy, consent, and potential stigmatization. Balancing data sharing for public health with individual rights is paramount.
9. Conclusion
The opioid and prescription drug abuse epidemic demands multifaceted solutions, and Health IT plays a pivotal role in this effort. Through comprehensive electronic records, real-time monitoring, decision support, telehealth, and data analytics, healthcare providers and policymakers can significantly reduce misuse, prevent overdoses, and improve patient safety.
However, realizing these benefits requires overcoming barriers such as interoperability, privacy concerns, and provider engagement. As technology advances, integrating innovative tools like AI and blockchain will further enhance our capacity to combat prescription drug abuse effectively.
The fight against this epidemic is ongoing, but with strategic deployment of Health IT, we can make substantial progress toward safer prescribing practices, better patient outcomes, and ultimately, a healthier society.
References and Further Reading
- Centers for Disease Control and Prevention (CDC). (2020). Understanding the Epidemic. https://www.cdc.gov/drugoverdose/epidemic/index.html
- U.S. Food and Drug Administration (FDA). (2018). Strategies to Address Prescription Drug Abuse. https://www.fda.gov/
- National Institute on Drug Abuse (NIDA). (2021). Prescription Drugs and Drug Misuse. https://www.drugabuse.gov/
- Office of the National Coordinator for Health Information Technology (ONC). (2019). Health IT and Opioid Crisis. https://www.healthit.gov/
- CDC’s Guide to Implementing a Prescription Drug Monitoring Program. (2017). https://www.cdc.gov/drugoverdose/resources/index.html